PDA,TOF,TGA,TAPVC
Posted by jobinmartin on August 2, 2010

In the developing fetus, the ductus arteriosus (DA) is the vascular connection between the pulmonary artery and the aortic arch that allows most of the blood from the right ventricle to bypass the fetus’ fluid-filled compressed lungs. During fetal development, this shunt protects the right ventricle from pumping against the high resistance in the lungs, which can lead to right ventricular failure if the DA closes in-utero.
When the newborn takes its first breath, the lungs open and pulmonary vascular resistance decreases. After birth, the lungs release bradykinin to constrict the smooth muscle wall of the DA and reduce bloodflow through the DA as it narrows and completely closes, usually within the first few weeks of life. In most newborns with a patent ductus arteriosus the blood flow is reversed from that of in utero flow, i.e. the blood flow is from the higher pressure aorta to the now lower pressure pulmonary arteries.
A patent ductus arteriosus allows a portion of the oxygenated blood from the left heart to flow back to the lungs by flowing from the aorta (which has higher pressure) to the pulmonary artery. If this shunt is substantial, the neonate becomes short of breath: the additional fluid returning to the lungs increases lung pressure to the point that the neonate has greater difficulty inflating the lungs. This uses more calories than normal and often interferes with feeding in infancy. This condition, as a constellation of findings, is called congestive heart failure. In some cases, such as in transposition of the great vessels (the pulmonary artery and the aorta), a PDA may need to remain open. In this cardiovascular condition, the PDA is the only way that oxygenated blood can mix with deoxygenated blood. In these cases, prostaglandins are used to keep the patent ductus arteriosus open.Without treatments, the disease may progress from left-to-right (noncyanotic heart) shunt to right-to-left shunt (cyanotic heart) called Eisenmenger syndrome.
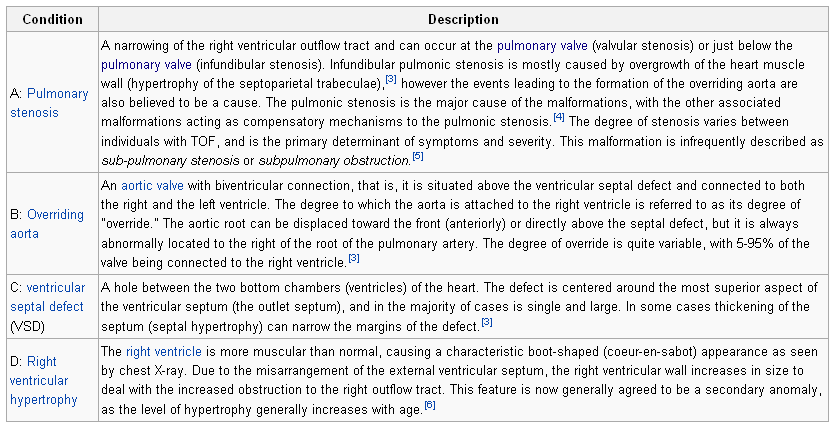
TOF

Tetralogy of Fallot results in low oxygenation of blood due to the mixing of oxygenated and deoxygenated blood in the left ventricle via the VSD and preferential flow of the mixed blood from both ventricles through the aorta because of the obstruction to flow through the pulmonary valve. This is known as a right-to-left shunt. The primary symptom is low blood oxygen saturation with or without cyanosis from birth or developing in the first year of life. If the baby is not cyanotic then it is sometimes referred to as a “pink tet”.Other symptoms include a heart murmur which may range from almost imperceptible to very loud, difficulty in feeding, failure to gain weight, retarded growth and physical development, dyspnea on exertion, clubbing of the fingers and toes, and polycythemia.
Children with tetralogy of Fallot may develop “tet spells”. The precise mechanism of these episodes is in doubt, but presumably results from a transient increase in resistance to blood flow to the lungs with increased preferential flow of desaturated blood to the body. Tet spells are characterized by a sudden, marked increase in cyanosis followed by syncope, and may result in hypoxic brain injury and death. Older children will often squat during a tet spell, which increases systemic vascular resistance and allows for a temporary reversal of the shunt.Oxygen is effective in treating spells because it is a potent pulmonary vasodilator and systemic vasoconstrictor. This allows more blood flow to the lungs.
Squatting
There are also simple procedures such as squatting and the knee chest position which increases aortic wave reflection, increasing pressure on the left side of the heart, decreasing the right to left shunt thus decreasing the amount of deoxygenated blood entering the systemic circulation.
The abnormal “coeur-en-sabot” (boot-like) appearance of a heart with tetralogy of Fallot is easily visible via chest x-ray
The Blalock-Taussig shunt (also referred to as a Blalock-Thomas-Taussig shunt) is a surgical procedure to give palliation to cyanotic heart defects which are common causes of blue baby syndrome. In modern surgery, this procedure is temporarily used to direct blood flow to the lungs and relieve cyanosis while the infant is waiting for corrective or palliative surgery.
One branch of the subclavian artery or carotid artery is separated and connected with the pulmonary artery. The lung receives more blood with low oxygenation from the body. The first area of application was tetralogy of Fallot.
TGA

Total Anomalous Pulmonary venous connection
Total anomalous pulmonary venous connection (TAPVC) consists of an abnormality of blood flow in which all 4 pulmonary veins drain into systemic veins or the right atrium with or without pulmonary venous obstruction. Systemic and pulmonary venous blood mix in the right atrium. An atrial defect or foramen ovale (part of the complex) is important in left ventricular output both in fetal and in newborn circulation.
Eisenmenger Syndrome
Eisenmenger’s syndrome (or Eisenmenger’s reaction) is defined as the process in which a left-to-right shunt caused by a ventricular septal defect in the heart causes increased flow through the pulmonary vasculature, causing pulmonary hypertension, which in turn, causes increased pressures in the right side of the heart and reversal of the shunt into a right-to-left shunt. Eisenmenger’s syndrome specifically refers to the combination of systemic-to-pulmonary communication, pulmonary vascular disease and cyanosis.
The left side of the heart supplies blood to the whole body, and as a result has higher pressures than the right side, which supplies only deoxygenated blood to the lungs. If a large anatomic defect exists between the sides of the heart, blood will flow from the left side to the right side. This results in high blood flow and pressure travelling through the lungs. The increased pressure causes damage to delicate capillaries, which then are replaced with scar tissue. Scar tissue does not contribute to oxygen transfer, therefore decreasing the useful volume of the pulmonary vasculature. The scar tissue also provides less flexibility than normal lung tissue, causing further increases in blood pressure, and the heart must pump harder to continue supplying the lungs, leading to damage of more capillaries.
The reduction in oxygen transfer reduces oxygen saturation in the blood, leading to increased production of red blood cells in an attempt to bring the oxygen saturation up. The excess of red blood cells is called polycythemia. Desperate for enough circulating oxygen, the body begins to dump immature red cells into the blood stream. Immature red cells are not as efficient at carrying oxygen as mature red cells, and they are less flexible, less able to easily squeeze through tiny capillaries in the lungs, and so contribute to death of pulmonary capillary beds. The increase in red blood cells also causes hyperviscosity syndrome.
A person with Eisenmenger’s Syndrome is paradoxically subject to the possibility of both uncontrolled bleeding due to damaged capillaries and high pressure, and random clots due to hyperviscosity and stasis of blood.
Eventually, due to increased resistance, pulmonary pressures may increase sufficiently to cause a reversal of blood flow, so blood begins to travel from the right side of the heart to the left side, and the body is supplied with deoxygenated blood, leading to cyanosis and resultant organ damage.
Cor Pulmonale
Cor pulmonale (Latin cor, heart + New Latin pulmōnāle, of the lungs) or pulmonary heart disease is enlargement of the right ventricle of the heart as a response to increased resistance or high blood pressure in the lungs.
Chronic cor pulmonale usually results in right ventricular hypertrophy (RVH), whereas acute cor pulmonale usually results in dilation.
Hypertrophy is an adaptive response to a long-term increase in pressure. Individual muscle cells grow larger and change to drive the increased contractile force required to move the blood against greater resistance.
Dilation is a stretching of the ventricle in response to acute increased pressure.
To be classified as cor pulmonale, the cause must originate in the pulmonary circulation system.
Nutmeg liver may result…
Leave a comment